Diabetes Wellness Guide
Optimizing your health and wellness while living with diabetes.
Diabetes is a lifelong, chronic condition where there is not enough insulin in the body to effectively assist with digestion after eating. Food is broken down during digestion into sugar.
Insulin is used to change the sugar and starches into energy that the body needs through the day. Without enough insulin, glucose builds up in the blood and is indicative of diabetes.
There are two types of diabetes:
- Type 1 Diabetes is an autoimmune condition where the body does not produce any insulin.
- Type 2 Diabetes is when the pancreas cannot make enough insulin, or the body has problems using the insulin.
Diabetes and High Blood Sugar
Tracking blood sugar levels are an important part of managing diabetes.
High blood sugar can harm many parts of the body, such as the eyes, heart, blood vessels, nerves, and kidneys. It can also increase your risk for other health problems and complications.
Suggested blood sugar levels for Type 1 and Type 2 diabetics is as follows:
Adults with Type 1 or Type 2 Diabetes
- Experts suggest an A1c of lower than 7% for most Type 1 and Type 2 diabetic adults. Before meals, the suggested target blood glucose range is 80 to 130 mg/dL. At one to two hours after meals, it is lower than 180 mg/dL.
- Pregnant Women: Experts suggest an A1c of 6.0% to 7.0% for diabetic pregnant women. Before meals, the target blood sugar range is less than 95 mg/dL. At two hours after meals, the range is less than 120 mg/dL.
Children Under 18
- Type 1 Diabetes: Experts suggest an A1c of lower than 7.5% for children. Before meals, the suggested target blood glucose range is 90 to 130 mg/dL. At bedtime and overnight, the suggested range is 90 to 150 mg/dL.
- Type 2 Diabetes: Experts suggest an A1c of lower than 7.0% for children. Before meals, the suggested target blood glucose range is 80 to 130 mg/dL. At one to two hours after meals, the suggested range is lower than 180 mg/dL.
Source: Healthwise
Managing Diabetes
Diabetes Management Tracker
Use this wallet tracker to keep your yearly diabetes care organized:
Diabetes Action Plan
Use this wallet tracker to keep your yearly diabetes care organized:
Tools and suggestions to help you thrive.
For those living with diabetes, there are several things that can be done to manage health problems caused by Type 1 and Type 2 diabetes, including:
Investing in self-care and healthy eating.
Make a list of what self-care practices you need to do every day to manage your diabetes, such as blood sugar checks, foot check, take medications, and physical activity.
Report to your doctor any change in symptoms. Be sure to ask questions if you do not understand. Make and keep up with all scheduled doctors’ appointments.
Healthy eating habits can help minimize the impacts of diabetes. Things you can do include managing your portions and balancing your plate with healthy and colorful foods.
Making healthy lifestyle choices.
For individuals with Type 1 and Type 2 diabetes, things you can do include:
- Take your medicine as your doctor told you
- Do health checks (including blood sugar checks) at home (as suggested by your doctor)
- Know your goal blood sugars
- Know how to treat low and high blood sugars
- Keep active and exercise
- Know the signs your condition is getting worse and inform your provider of changes
- Maintain a healthy weight
- Practice healthy eating habits
- Make and keep all your doctor's appointments; ask questions if you don't understand instructions you are provided
Maintaining and supporting your best health.
If you’d like to learn more about either a new diagnosis or a chronic condition such as diabetes that you’ve had for a while, Martin’s Point has a team of nurse care managers who are here to help. This service is offered at no cost to you.
A nurse care manager helps you learn about your chronic conditions and build skills to proactively manage your health. They review medications, help coordinate your care, and find helpful community resources.
If you want to speak to a care manager, call: 1-877-659-2403
Diabetes Treatment
The diagnosis of diabetes can come with many unknowns and concerns about what to do next.
Your provider will tell you how often they would like to see you to monitor your diabetes. At a minimum you should have yearly monitoring at your Medicare Annual Wellness Visit and/or annual physical exam.
Below you will find additional information on the management and treatment of diabetes, including monitoring, medication information, as well as tips for minimizing the risk of heart disease for individuals with diabetes.
Below is recommended monitoring that should be performed yearly for patients who have known type 1 or type 2 diabetes.
Medicare Annual Wellness Exam
For those on Medicare, this is the most important doctor visit of the year. This is a visit for you to update your personalized prevention plan and discuss any chronic conditions and monitoring needs.
Hemoglobin A1c
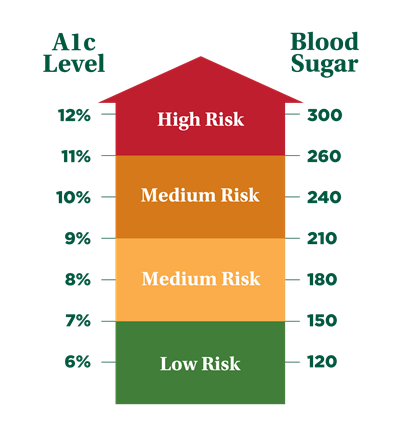
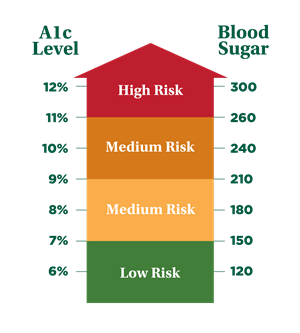
This blood test gives a picture of your average blood sugar level over the past three months. A1c results are represented as a percentage and each percentage relates to an average blood sugar level. The higher the A1c level, the greater your risk of developing complications (see chart at right).
Talk with your doctor about your numbers—for most people, the A1c goal is 7 or below but this may vary based on age and health conditions (American Diabetes Association). Your provider will determine your A1c goal and how often you’ll have your A1c tested. It’s not uncommon to have it tested twice a year if you are meeting your A1c goal; this test may be performed more frequently if your A1c is not in range.
Kidney Disease
Kidney disease is one of the common complications of diabetes, especially in those whose A1c levels are difficult to control. One of the ways your provider can monitor your kidney health is yearly blood work and urine tests. A common blood test for your kidneys is the estimated glomerular filtration rate (eGFR) and a common urine test is the urine albumin creatinine ratio (uACR). These tests may be performed more frequently than yearly if you show evidence of kidney disease.
Hypertension
Hypertension is when the force of blood pushing against the blood vessel walls is consistently too high. Nearly half of adults have high blood pressure (readings above 130/80) and half of those have uncontrolled blood pressure (readings above 140/90)). High blood pressure often doesn’t have symptoms but can increase your risk of heart attacks and strokes. Often your doctor will prescribe medications and monitoring to lower your blood pressure. Check out our Heart and Vascular Health page to learn more ways to control high blood pressure.
Eye Disease
Eye disease is a common complication of diabetes. A disease of the eye called retinopathy can happen. Retinopathy is when the retina develops a hole and can lead to blindness in one or both eyes. A yearly dilated-eye exam is recommended for all patients with diabetes. Finding and treating this condition early can help maintain your eyesight.
Neuropathy
Neuropathy is damage to the peripheral nervous system, often experienced in the legs and feet resulting in loss of sensation or pain. In addition to foot checks performed at home, this can be monitored by regular foot exams at your provider’s office during your Medicare Annual Wellness Visit, your annual physical exam, or diabetic visit. During this foot exam, your doctor will look for any concerning wounds, check sensation, and look for any discoloration which may be a sign of concern.
You may be prescribed any one of these medications to treat your diabetes. Always be sure you get specific information on the medicine you're taking.
For a full list of side effects, check the information that came with the medicine you're using. If you have questions, talk to your pharmacist or doctor.
Insulin Medications
Insulin helps keep your blood sugar level tightly controlled and within a target range. It can be taken by an injection or through an insulin pump. Rapid-acting insulin is also available as a powder that you inhale. The amount and type of insulin you need changes over time, depending on age, hormones (such as during rapid growth or pregnancy), and changes in exercise routine. You may need higher doses of insulin during times of illness or emotional stress.
Know the dose of each type of insulin you take, when you take the doses, how long it takes for each type of insulin to start working (onset), when it will have its greatest effect (peak), and how long it will work (duration).
Never skip a dose of insulin without the advice of your doctor.
Non-Insulin Medications
Non-insulin medicines for diabetes help you control blood sugar. Each type works in a different way to help you control your blood sugar. For example, some types of non-insulin medicines help your body make insulin to lower your blood sugar. Others lower how much insulin your body needs. Some types can slow how quickly your body digests sugars or can remove extra glucose through your urine.
Medications to Help Reduce the Risk of Heart Disease in Diabetic Patients
Over time, high blood sugar can cause damage to blood vessels and nerves. This can increase the risk for cardiovascular disease, which includes heart disease, stroke, and blood vessel damage. Controlling blood sugars, following recommended lifestyle changes, and using preventive medications can all help to reduce the risk for heart disease. Additionally, controlling other risk factors for heart disease, such as high blood pressure and high cholesterol, can help to reduce the risk of heart disease events, including heart attack and stroke.
As always, it is recommended that you speak with your provider before adding new medications and to determine if additional therapy is recommended for you.
Medications commonly used in diabetes to prevent cardiovascular complications include:
Medications |
|
|---|---|
|
Aspirin |
Depending on your history and individual risk factors, your doctor may recommend you take aspirin daily. Aspirin helps prevent blood clots from forming and can reduce the risk of heart attack and stroke. Ask your doctor before starting aspirin therapy on your own. |
| Statin Medications (HMG-CoA Reductase Inhibitors) |
In diabetic patients with cardiovascular disease, statin therapy should usually be added to lifestyle changes regardless of cholesterol levels. For patients without cardiovascular disease, you and your doctor should discuss whether taking a statin medication is a good choice given your individual risk factors. Typically, diabetic patients 40 years of age and older will be on statin therapy to help control cholesterol. |
| ACE Inhibitors, ARBs (Renin-Angiotensin System Inhibitors) |
For diabetics with kidney disease and high blood pressure, taking ACE inhibitors (angiotensin-converting enzyme) or ARBs (angiotensin receptor blockers) may be beneficial, as these medications may slow kidney disease progression while working to lower blood pressure.
|
Chronic Disease and Your Mental Health
A chronic disease is one that restricts your daily life and/or requires medical attention for at least one year.
Conditions like diabetes, coronary artery disease, peripheral artery disease, atrial fibrillation, and cerebrovascular disease are just some examples of chronic diseases.
For many, having a chronic disease can cause major disruption in one’s previous routine. Some people need to take new medications, eat differently, and/or perform routine monitoring at home. Some may have more doctors’ appointments or health care expenses. Some may worry about experiencing another heart attack or stroke or their condition worsening. Because of the nature of chronic diseases, there is an increased likelihood of mental health issues like anxiety or depression.
If you are experiencing symptoms of depression or anxiety, please speak with your health care provider. These conditions are common, and your doctor will know how to best support you. Untreated, conditions like anxiety and depression can worsen and can also become a barrier to managing your chronic disease. Some people experiencing anxiety or depression may have difficulty going to their doctors’ appointments, taking their medications, or following the other prescribed lifestyle changes that help manage their chronic condition.
Please check out our Mental Health webpage to learn more.